Phimosis is a medical condition characterized by the inability to fully retract the foreskin over the head (glans) of the penis. While it is common in infants and young boys, it can persist into adulthood or develop later due to various factors. Understanding the causes, symptoms, diagnosis, and treatment options for phimosis is essential for those affected, as it can lead to discomfort, infections, and complications if left untreated. This blog provides a comprehensive overview of phimosis, including insights into phimosis treatment in India and advanced procedures like ZSR circumcision in India.
What is Phimosis?
Phimosis occurs when the foreskin, a retractable layer of skin covering the glans of the penis, is too tight to be pulled back. This condition is normal in newborns and young children, where the foreskin is naturally fused to the glans at birth. In most cases, this resolves by adolescence as the foreskin gradually separates and becomes retractable. However, when phimosis persists or develops in adulthood, it may require medical attention.
There are two primary types of phimosis:
- Physiological Phimosis: This is a normal developmental condition in infants and young boys. The foreskin is naturally non-retractable due to adhesions between the foreskin and glans. It typically resolves on its own by age 5–7 without intervention.
- Pathological Phimosis: This occurs due to scarring, infection, or inflammation, often in older children or adults. It does not resolve naturally and may require medical or surgical treatment.
Causes of Phimosis
Phimosis can result from a variety of factors, depending on whether it is physiological or pathological. Common causes include:
- Natural Development: Physiological phimosis is common in newborns and young boys due to natural adhesions between the foreskin and glans. These adhesions typically break down over time.
- Infections: Recurrent bacterial or fungal infections, such as balanitis (inflammation of the glans) or balanoposthitis (inflammation of both the glans and foreskin), can cause scarring and tightening of the foreskin.
- Poor Hygiene: Inadequate cleaning of the penile area can lead to the buildup of smegma, bacteria, or other substances, increasing the risk of infections and phimosis.
- Injury or Trauma: Forceful retraction of the foreskin or injury to the penile area can cause scarring, leading to pathological phimosis.
- Skin Conditions: Conditions like lichen sclerosus, eczema, psoriasis, or lichen planus can cause inflammation and scarring, contributing to foreskin tightness.
- Medical Conditions: Diabetes can increase the risk of infections and phimosis due to higher susceptibility to fungal infections.
- Frenulum Breve: A short or tight frenulum (the band of tissue connecting the foreskin to the glans) can restrict foreskin movement.
Symptoms of Phimosis
The symptoms of phimosis can vary depending on its severity and underlying cause. In mild cases, individuals may experience no symptoms, while severe cases can lead to significant discomfort. Common symptoms include:
- Difficulty Retracting the Foreskin: The hallmark sign of phimosis is the inability to pull the foreskin back over the glans, either partially or completely.
- Pain or Discomfort: Pain may occur during urination, erections, or sexual activity due to the tight foreskin.
- Swelling and Redness: The foreskin may appear swollen, red, or tender, especially if an infection is present.
- Recurrent Infections: Difficulty cleaning under the foreskin can lead to bacterial or fungal infections, such as balanitis or balanoposthitis.
- Urinary Problems: A tight foreskin can restrict urine flow, causing a weak stream, difficulty urinating, or urinary tract infections (UTIs).
- Painful Erections: Severe phimosis can cause pain or discomfort during erections, potentially affecting sexual function.
- Paraphimosis: A related condition where the foreskin is retracted but cannot return to its original position, leading to painful swelling. This is a medical emergency.
If left untreated, phimosis can lead to complications such as chronic infections, penile pain, sexual dysfunction, or, in rare cases, penile cancer.
How to Diagnose Phimosis
Diagnosing phimosis typically involves a straightforward process conducted by a urologist or healthcare provider. The diagnostic steps include:
- Medical History: The doctor will ask about symptoms, medical history, previous infections, injuries, or conditions like diabetes that may contribute to phimosis.
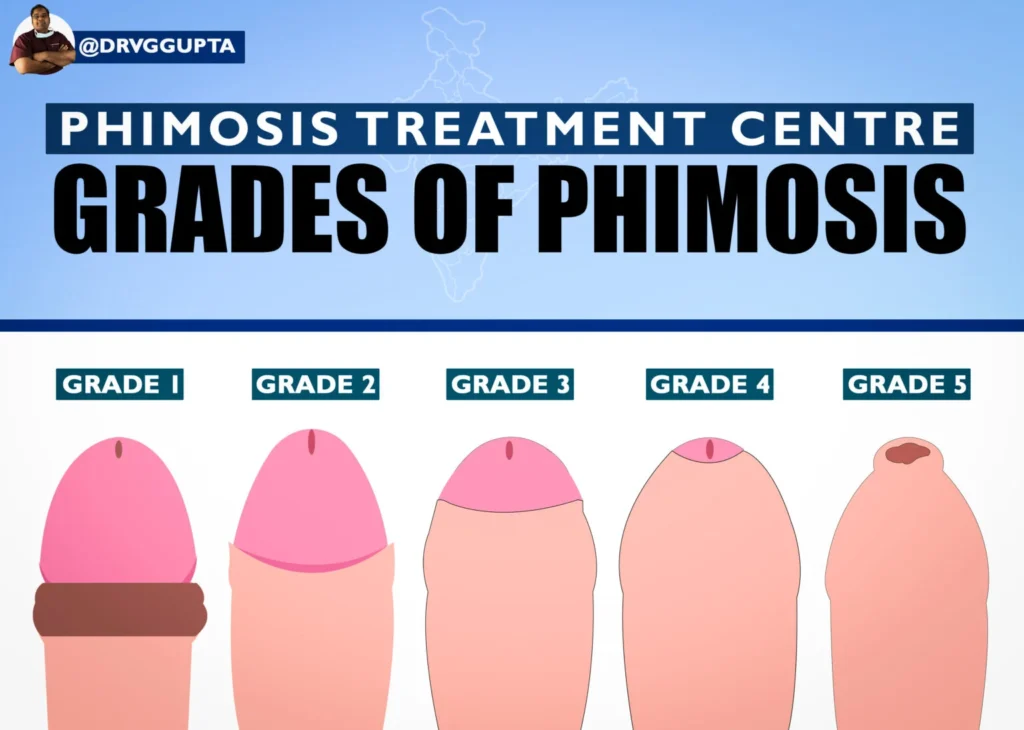
- Physical Examination: A visual and physical inspection of the penis and foreskin is usually sufficient to confirm phimosis. The doctor assesses the degree of foreskin retraction and checks for signs of infection, scarring, or inflammation.
- Additional Tests: In some cases, diagnostic tests may be ordered to rule out underlying causes, such as:
- Urine Tests: To check for urinary tract infections.
- Swab Tests: To identify bacterial or fungal infections in the foreskin.
- Blood Tests: To measure blood sugar levels if diabetes is suspected.
Accurate diagnosis is crucial to differentiate between physiological and pathological phimosis and to determine the appropriate treatment plan.
Treatment Options for Phimosis
Treatment for phimosis depends on its severity, cause, and the patient’s age and preferences. Options range from non-surgical methods to surgical interventions. Below are the primary treatment approaches:
Non-Surgical Treatments of Phimosis
- Topical Steroid Creams:
- Description: Steroid creams, such as betamethasone, are applied to the foreskin to reduce inflammation and promote elasticity. These are typically used for mild to moderate cases of phimosis.
- How It Works: The cream is applied 2–3 times daily for several weeks, often combined with gentle stretching exercises to loosen the foreskin.
- Effectiveness: Effective in many cases, especially for physiological phimosis, with minimal side effects. However, results vary, and long-term use of steroids should be avoided.
- Considerations: Patients should follow medical guidance to avoid complications like skin thinning.
- Manual Stretching Exercises:
- Description: Gentle, controlled stretching of the foreskin over time can help loosen it.
- How It Works: The foreskin is pulled back gradually, avoiding pain or forceful retraction, often in combination with steroid creams.
- Effectiveness: Suitable for mild cases but requires patience and consistency. Incorrect techniques can worsen the condition or cause paraphimosis.
- Considerations: Should be done under medical supervision to prevent injury.
- Ayurvedic Treatments:
- Description: Some clinics, such as Sidri International Skin Hair and Sexology Clinic in Delhi, offer non-surgical Ayurvedic treatments for phimosis. These may involve herbal remedies, oils, or exercises to reduce inflammation and improve foreskin flexibility.
- How It Works: Treatments aim to balance the body’s energies (doshas) and promote healing without surgery.
- Effectiveness: Anecdotal evidence suggests success in mild cases, but scientific data is limited. Patients should consult qualified practitioners.
- Dilation:
- Description: Medical tools are used to gradually widen the foreskin opening under supervision.
- How It Works: Performed by a healthcare provider, this method stretches the foreskin without surgical intervention.
- Effectiveness: Useful for mild cases but less common than other non-surgical options.
Surgical Treatments of Phimosis
- Circumcision:
- Description: Circumcision involves the surgical removal of the foreskin, exposing the glans. It is a permanent solution for phimosis and is recommended for severe or recurrent cases.
- Types of Circumcision:
- Traditional Circumcision: The foreskin is cut using a scalpel or surgical scissors, and the edges are stitched with dissolvable sutures.
- Laser Circumcision: A high-energy laser beam is used to cut the foreskin, offering precision, minimal bleeding, and faster recovery.
- ZSR Circumcision (Stapler Circumcision): A modern technique using a disposable stapler device to cut and seal the foreskin in one motion. It is bloodless, stitchless, and quick, with a recovery time of 7–10 days. ZSR circumcision in India is gaining popularity, with specialists like Dr. Vijayant Govinda Gupta in Delhi offering this advanced procedure.
- Procedure: Performed under local or general anesthesia, circumcision takes 10–30 minutes, depending on the technique. The patient is positioned comfortably, and the surgical area is sterilized to prevent infection.
- Recovery typically takes 1–2 weeks, with full healing occurring within 4–6 weeks. Patients are advised to keep the area clean, apply ointments, and avoid sexual activity or strenuous exercise during recovery.
- Benefits: Eliminates phimosis, reduces the risk of infections, improves hygiene, and lowers the risk of penile cancer and certain STIs.
- Risks: Includes pain, bleeding, infection, or anesthesia-related complications, though these are rare (approximately 2% of cases).
- Preputioplasty:
- Description: A less invasive surgical option where small incisions are made in the foreskin to widen it, preserving the foreskin.
- Procedure: Performed under local or general anesthesia, it involves making incisions to relieve tightness without removing the foreskin.
- Recovery: Similar to circumcision, but may heal faster due to less tissue removal.
- Benefits: Preserves the foreskin, which some patients prefer for aesthetic or functional reasons.
- Risks: Less common than circumcision, with a small risk of recurrence if scarring persists.
How to Prevent Phimosis
While physiological phimosis cannot be prevented, pathological phimosis can be minimized through proper care:
- Maintain Good Hygiene: Regularly clean the penis with mild soap and water, gently retracting the foreskin as far as comfortable.
- Avoid Forceful Retraction: Forcing the foreskin back can cause trauma and scarring.
- Manage Underlying Conditions: Control diabetes and treat infections promptly to reduce the risk of phimosis.
- Wear Comfortable Clothing: Loose, breathable underwear prevents moisture buildup, reducing infection risk.
- Regular Checkups: Consult a urologist for persistent foreskin issues, especially if symptoms like pain or infections occur.
Visit Our Men’s Health Website

Phimosis is a manageable condition with a range of treatment options, from non-surgical methods like steroid creams and stretching exercises to surgical procedures like circumcision and preputioplasty. Early diagnosis and proper care are key to preventing complications and improving quality of life. For those seeking phimosis treatment in Delhi, advanced options like ZSR circumcision in India offer safe, effective, and minimally invasive solutions. Consult a qualified urologist or specialist to determine the best approach for your condition, and prioritize hygiene to maintain penile health.
If you’re experiencing symptoms of phimosis or seeking treatment, clinics in Delhi, Dr. Vijayant Govinda Gupta’s Clinic, New Delhi Andrology Center, provide expert care tailored to your needs. Book a consultation today to explore your options and take the first step toward a pain-free life.